We ♥ PrEP, PEP, & DoxyPEP
HIV medications have been tremendously successful in keeping people living with HIV healthy. They’re also extremely effective at stopping new HIV infections. We are now seeing that antibiotics used to treat STIs are also effective at preventing them before they start. Here’s information about preventing HIV and STIs using medications.
PrEP (for HIV)
What is PrEP?
PrEP stands for Pre-Exposure Prophylaxis. PrEP is an effective way to prevent HIV infection. Currently, there are two methods of PrEP approved by the U.S. Food and Drug administration (FDA)– daily oral PrEP pills (taking one Truvada or Descovy pill every day) and bi-monthly injectable PrEP (cabotegravir). Studies (iPrEx study and iPrEx OLE study) show that PrEP can reduce the risk of HIV infection by 92-99% when taken as prescribed by your healthcare provider.
Non-daily PrEP 2-1-1 for Truvada (or “on-demand PrEP”) also has been shown to be effective; see below for more information. There is no evidence yet of PrEP 2-1-1 with Descovy being effective.
Who is PrEP for?
PrEP is for HIV-negative people who may be exposed to HIV through sex or injection drug use. According to the U.S. Centers for Disease Control and Prevention (CDC), PrEP should be considered for all adults and adolescents (weighing 77 pounds or more) who are HIV-negative and who sexually-active and/or injecting drugs. This is because anyone of any gender or age can be vulnerable to HIV based on their sex lives or drug use practices.
The CDC recommends PrEP especially for people who’ve had anal or vaginal/front hole sex in the past 6 months AND any of the following:
- A sex partner living with HIV (especially if your partner has an unknown or detectable viral load)
- Bacterial STI–like gonorrhea or chlamydia–in the past 6 months
- Past or current condomless sex with a partner
There are also differences for who can take certain medications for PrEP based on available research data:
- Truvada (oral pill): Anyone on Truvada can take it daily to prevent HIV transmission during sex and injection drug use. If you are a cisgender man, you may be able to use it before you have sex using PrEP 2-1-1 dosing. (Read more about it below under “What is PrEP 2-1-1?”)
- Descovy (oral pill): Descovy is approved to reduce the risk of HIV transmission during sex, except for those who have receptive front hole/vaginal sex.
- Cabotegravir (injectable): Cabotegravir is approved for use as HIV prevention during sex for people weighing at least 77 pounds, regardless of gender. Injectable PrEP users will need to receive an injection from a healthcare provider every week for four weeks and then get an injection every two months.
How do I start and stay on PrEP?
To start oral PrEP, you will need to:
- See a healthcare provider who will ask you questions about your sex life and substance use. If your provider doesn’t ask you about them, it’s best to start the conversation.
- Get a blood test for HIV (since you have to be HIV-negative to use PrEP) and Hepatitis B & C*
- Get a kidney function test (part of your blood test)
- Get a full STI screening (gonorrhea, chlamydia, syphilis)
- Get a lipid panel blood test (only if you’re taking Descovy)*
These tests can typically all be done at the same appointment. You may be able to start oral PrEP the same day you have your appointment.
To stay on oral PrEP, you will need to:
- Get tested for HIV and STIs every three months
- Get a kidney test once a year (if you’re under 50) and every six months (if you’re 50+ years old)
- Get tested for Hepatitis C once a year
If you ever stop taking oral PrEP or decide to take PrEP on-demand (PrEP 2-1-1), let your healthcare provider know so you can get the right lab tests done.
To start injectable PrEP, you will need to:
- See a healthcare provider who will ask you questions about your sex life and substance use. If your provider doesn’t ask you about them, it’s best to start the conversation.
- Get a blood test for HIV (since you have to be HIV-negative to use PrEP)
- Get a full STI screening (gonorrhea, chlamydia, syphilis)
- Some doctors may start you on a course of daily oral PrEP called an “oral lead-in.” This makes it easy for people who don’t react well to the drug to stop taking it immediately so that their side-effects go away.
- Receive your first injection.
To stay on injectable PrEP, you will need to:
- If you did a month of oral lead-in, your second shot will be two months after your first. Otherwise, your second shot will be a month after the first and every two months after that.
- Take an HIV blood test at every appointment where you receive your injections.
- Depending on the type of sex you have, you may need to receive STI/STD screenings at your follow up visits.
If you decide to stop taking injectable PrEP, let your healthcare provider know so that they can help you get the right testing done.
How effective is PrEP?
The simplest answer: very. And the more you follow the recommendations, the better it works. Studies show that daily oral PrEP, injectable PrEP, and PrEP 2-1-1 (where you take two pills before sex, then one pill each day for the next 48 hours) are all effective. See your healthcare provider every three months for an evaluation and lab testing that includes comprehensive STI screening.
There have been a very few PrEP failures, in which people have gotten HIV despite following the recommendations. However, these are extremely rare (fewer than a dozen cases in the US to date).
In studies, injectable cabotegravir was more effective than oral PrEP. This is because the injections are long-acting and it’s more difficult to miss doses.
PrEP does not protect people from any sexually transmitted infections (including gonorrhea, chlamydia, syphilis, and herpes).
Health organizations recommend that for the most effective HIV prevention, people who take PrEP combine it with other safe sex strategies – like using condoms and using your own needs and works when injecting drugs.
Also, it’s important to note that daily PrEP doesn’t begin working immediately. When you start taking daily PrEP, it takes at least:
- 7 days for the drug to become effective at preventing HIV if you’re having anal sex
- 20 days for the drug to become effective at preventing HIV if you’re having vaginal/front hole sex
- Injectable cabotegravir will become effective at preventing HIV seven days after the first shot.
If you intend to stop oral PrEP, you should keep on taking it for at least four weeks after you last had sex or injected drugs.
Side effects of PrEP
There are relatively few side-effects reported by people taking PrEP. These vary by which type or PrEP you use.
If you’re taking oral pills (Truvada or Descovy): Some people report experiencing “start-up syndrome” when they begin PrEP. This can include nausea, headache, loss of appetite, and diarrhea. Usually, symptoms are mild and stop after the first month.
If you have Hepatitis B and stop taking DESCOVY, your Hepatitis B may suddenly get worse. Do not stop taking DESCOVY without first talking to your healthcare provider, as they will need to check your health or give you medicine to treat your Hepatitis B.
Truvada-based PrEP is also associated with small decreases in bone mineral density (bone strength) in some people. People with greater bone density are less likely to suffer from broken bones or fractures after injury, which is why decreases in bone density is important. Decreases in bone strength are usually small, and not associated with fractures or broken bones; bone density increases again after people stop taking Truvada. Descovy based PrEP may cause increases in cholesterol and weight.
PrEP may also affect your kidneys. Following-up with your healthcare provider every three months is important so that they can perform lab testing to ensure your kidneys are working properly and to determine if you should stop taking PrEP for the time being.
For more information on the differences between Truvada and Descovy, click here.
If you’re taking injectable PrEP (Cabotegravir): Injectable PrEP’s main additional side-effect is pain and redness at the injection site. This can occur alongside other possibilities, like diarrhea, headache, and raised liver enzymes. If your doctor is worried about side-effects, you may start on a course of oral PrEP called an “oral lead-in.” This makes it easy for people who don’t react well to the drug to stop taking it immediately so that their side-effects go away.
Where to get PrEP
People can get PrEP in a number of different ways. If you are currently in medical care and have medical insurance, you can talk to your regular healthcare provider about PrEP.
You can also look for PrEP-friendly medical providers at PrEPLocator.org (U.S.) or start with our global testing resources to find a clinic who may answer questions about PrEP access in your country.
LGBT health centers or local HIV/AIDS service organizations in your area may also have PrEP services or have recommendations on how to access PrEP. Reach out to your local LGBT center or HIV/AIDS service agencies for more information.
In addition, Gilead Sciences (the manufacturer of Truvada and Descovy) has an Access to Medicines program.
How to afford PrEP
If you have health insurance, you can expect to pay the normal co-pay for a brand-name drug for oral PrEP. This cost varies from plan to plan.
Without insurance, PrEP is not cheap. It can cost thousands of dollars every year. But there are ways to get Truvada for PrEP at no or low cost. A number of U.S. states have established their own PrEP Assistance Programs. Most cover out-of-pocket expenses for the medication for insured patients and almost all programs cover the cost of clinical visits and lab tests regardless of health insurance coverage. In addition, Gilead Sciences (the manufacturer of Truvada) has a prescription assistance program.
Another option is to participate in a clinical research study or demonstration project of PrEP. You can search for PrEP studies that are now enrolling across the U.S. on the AVAC website.
What is PrEP 2-1-1?
PrEP 2-1-1 is named for a particular PrEP dosing schedule:
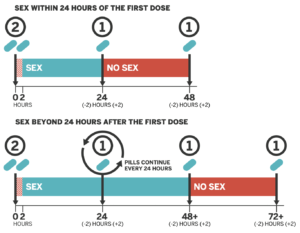
Image: San Francisco AIDS Foundation
- 2 pills are taken 2 to 24 hours before sex
- 1 pill 24 hours after the initial dose
- 1 final pill 24 hours later.
PrEP 2-1-1 is also known as “on-demand,” “event-driven,” “sex-driven” and “intermittent” PrEP. It is important to know that to date, only oral Truvada has been shown to be effective for PrEP 2-1-1. Studies are currently taking place to determine if Descovy is as well, but we do not yet have conclusive data.
How effective is PrEP 2-1-1?
The most well-known study, named IPERGAY, showed that PrEP 2-1-1 reduced risk of HIV infection by 86% compared to placebo. The continuation of the study provided a real-world look at how people use PrEP 2-1-1. This part of the study found that PrEP 2-1-1 reduced risk of HIV infection by 97%. Among those people having sex less frequently, there were zero HIV infections.
PrEP 2-1-1 has only been studied as an option for cisgender men who have anal sex with cisgender men, but only for those taking Truvada and those without active hepatitis B infection. PrEP 2-1-1 is not currently recommended for anyone else outside of cisgender men who have sex with cisgender men at this time.
It is important to note, however, that PrEP 2-1-1 is neither endorsed by the CDC, nor approved by the FDA, and is considered “off-label” use.
Overall, PrEP 2-1-1, when used correctly, can be an effective way to prevent HIV infection.
Who might benefit from PrEP 2-1-1?
While daily PrEP is currently the recommended way to take PrEP, PrEP 2-1-1 provides an alternative dosing strategy for cisgender gay men who would benefit from PrEP but find it hard to take a pill every day. It may be an option if you are able to anticipate when you’ll next have sex, and can take your pre-sex dose of PrEP 2 hours (preferably 24 hours) before then, and daily doses of PrEP for 48 hours after your last sexual encounter.
Who should not take PrEP 2-1-1?
PrEP 2-1-1 is only recommended for people having anal sex, since the drug may not be present at levels high enough if using PrEP 2-1-1 to protect vaginal tissues. PrEP 2-1-1 has not been adequately studied in cisgender women, cisgender men who have sex with cisgender women, transgender men, transgender women, people who inject drugs, or people who take Descovy for PrEP or use injectable PrEP. Furthermore, PrEP 2-1-1 is not recommended if you’re living with chronic hepatitis B.
In addition, if you are not able to anticipate when you have sex and cannot take your pre-sex dose of PrEP at least 2 hours (and preferably closer to 24 hours) before sexual activity, 2-1-1 PrEP may not be right for you. If you can’t always plan ahead and take your pre-sex dose at least two hours ahead, or remember to take a second and third dose afterwards, you may instead benefit from daily use.
Whatever your decision is about PrEP, or PrEP 2-1-1, be sure to ask your healthcare provider.
If you switch between 2-1-1 and daily PrEP use, you should retest for HIV prior to restarting if you’ve had sex when you haven’t been taking PrEP.
What is injectable PrEP?
In addition to PrEP that is taken orally, it’s now possible to take PrEP as a series of regularly scheduled injections. Cabotegravir has been shown in studies to be even more effective than oral PrEP because it’s long-acting and it’s harder to miss doses. It can lighten our mental load by taking one task off our daily to-do lists.
If your doctor is concerned about side-effects, which can include diarrhea, headache, and raised liver enzymes, along with injection site pain, you may start on a one month regimen of daily oral PrEP called an “oral lead-in.” If so, you’ll have an injection the following month and continue every other month after that. Otherwise, you’ll get your second injection a month after your first and then continue every other month after that.
There’s a growing body of research showing that injectable PrEP options are particularly effective for certain groups, including people having vaginal sex.
Resources
Want to learn more about PrEP? Check out these short videos and other resources. You’ll get a quick overview of what PrEP is, how well it works, and how to figure out if it may be right for you.
About PrEP
- PrEP Info: From the CDC
- Is PrEP Right for Me? Video by Greater than AIDS
An HIV doctor answers real-life questions about PrEP - BHOC Gay Men’s Sexual Health Partnership With Daddyhunt includes PrEP PSAs
- PrEP Medication Guide: From the CDC
- This brochure provides information on how PrEP prevents HIV, its side effects and safety, paying for PrEP, and available resources.
- What to Know About Truvada: From HIV.gov
- What to know about Descovy: From HIV.gov
- Is PrEP For You? Harlem United
Q&A about PrEP and “PrEP conversations” videos.
Paying for PrEP
- PrEP Medical Assistance Program: From Gilead Sciences
Gilead provides a medication assistance program for people taking PrEP who need help paying for the medication. Get info on how to apply and how to get covered. - State PrEP Financial Assistance Programs: From NASTAD
A list of U.S. state resources to help you cover the cost of PrEP.
For Your Healthcare Provider
Find a PrEP provider in your area and see if they take insurance or offer no-cost services.
The CDC makes a variety of resources available about PrEP including fact sheets, brochures, and videos.
It’s really important that people living with HIV do not to take PrEP. If you’ve recently started taking PrEP, and are worried that you’ve recently contracted HIV (either right before, or right after you started PrEP), find out what to do.
This resource was last updated March 18, 2025.
PEP (for HIV)
You can prevent HIV by taking medications called Post-Exposure Prophylaxis (PEP). PEP must be started within 72 hours (3 days) of when you were potentially exposed (like having condomless sex or sharing syringes) to prevent infection. Find where to get PEP near you here.
What is PEP?
PEP stands for Post-Exposure Prophylaxis. PEP prevents HIV infection in people who have been recently exposed to HIV. If you are HIV-negative but recently had condomless sex with someone whose HIV status you didn’t know, for example, consider taking PEP to prevent a possible HIV infection. If you have HIV, and think there’s a chance you exposed someone else to HIV, you can tell that person about PEP.
PEP is a four-week course of anti-HIV medications that prevent HIV infection. In order for PEP to work, it has to be started as soon as possible after the HIV exposure event.
That means if you think you’ve been exposed to HIV, and want to start taking PEP, do so as soon as possible. PEP has to be started within 72 hours (3 days) in order to work.
Should I go on PEP?
If you’re HIV-negative, not on PrEP, and your answer to any of the questions below is yes, talk to your doctor right away.
- Did you bottom without a condom with someone who is either HIV-positive and not undetectable or someone whose HIV status you don’t know?
- Did the condom break and you got a load up your butt?
- Did you top someone without a condom who is either HIV-positive and not undetectable or someone whose HIV status you don’t know?
- Have you shared needles with someone?
What is PEP for?
PEP is for HIV-negative people who may have been exposed to HIV during a single event. PEP is not a substitute for other proven HIV prevention methods, such as correct and consistent condom use, PrEP (pre-exposure prophylaxis), or use of sterile injection equipment.
How does PEP work?
You have to start PEP within 72 hours of exposure for PEP to work. Seek PEP right away if you think you’ve been exposed to HIV and you are not on PrEP. Your doctor will determine what treatment is right for you based on how you may have been exposed to HIV.
PEP consists of three antiretroviral medications that are taken for 28 days. PEP is safe but may cause side effects like nausea in some people. These side effects can be treated and are not life threatening. PEP is not 100% effective; it does not guarantee that someone exposed to HIV will not become infected with HIV.
What happens after I start PEP?
Make sure you take your meds. PEP does not work if you do not take the medications.
Continue to use condoms with sex partners while taking PEP and do not use injection equipment that has been used by others. This will help avoid spreading the virus to others if you become infected.
Return to your healthcare provider for more HIV testing one month, three months, and six months after the potential exposure to HIV. Your healthcare provider will give you a follow-up schedule.
Adapted from SFAF
DoxyPEP (for Chlamydia, Gonorrhea, & Syphilis)
Find doxyPEP here.
What is doxyPEP?
DoxyPEP stands for doxycycline post-exposure prophylaxis, a new way to decrease the chance of getting a bacterial sexually transmitted infection (STI).
Doxy is shorthand for doxycycline, a common antibiotic used to treat bacterial infections. You may have taken it for a skin condition or after you got diagnosed with a bacterial STI in the past.
Post-exposure prophylaxis means that a person receives treatment after an exposure. With doxyPEP, someone can take doxycycline following oral, anal, and vaginal/front hole sex.
The difference between doxyPEP and getting treated for an STI comes down to two main things:
- You’re taking treatment medications before you have symptoms
- You’re taking treatment medications before you test positive for an STI
Doing so reduces the chance that the bacteria in your body would cause an STI.
Which STIs does doxyPEP prevent?
DoxyPEP has been shown to prevent three major STIs: chlamydia, gonorrhea, and syphilis in cisgender men and transgender women, mostly having anal and oral sex.
While doxyPEP does not prevent HIV, there are two options for people who want to reduce their HIV risk: HIV PrEP (taken before sex or potential exposure to HIV) or HIV PEP (taken after sex or potential exposure to HIV).
Using condoms & lube are still an effective way to reduce your chance of getting HIV and other STIs. Find out how to prevent other STIs here.
How do I use doxyPEP?
A person takes 200mg of doxycycline up to 72 hours after they have oral, anal, or vaginal/front hole sex. It’s better to take it within 24 hours after sex, but you can take it up to 72 hours after. Doxycycline is safe to take daily if you’re having frequent sex.
Remember, the current guidance for doxyPEP is to take medications after sex, not used before sex like PrEP for HIV. We don’t yet know if taking doxycycline daily or before sex has any added benefit for preventing STIs like we do for HIV PrEP. Research studies are currently underway to determine if daily DoxyPrEP is effective at preventing bacterial STIs.
How effective is it?
A research study that enrolled cisgender men who have sex with men and transgender women in San Francisco and Seattle showed that doxyPEP decreased the risk of bacterial STIs by an average of 65%. However, the efficacy of doxyPEP in this study by the STI and the HIV status of participants.
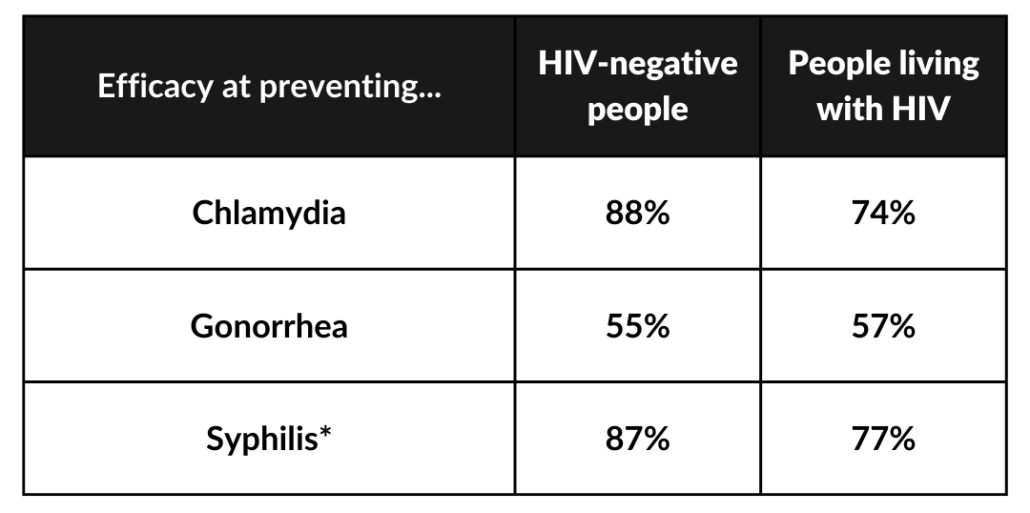
*In the studies, the number of syphilis infections was so small they couldn’t make broad statements about its efficacy for everyone.
Who can use doxyPEP?
If you are a cisgender man or transgender woman, doxyPEP is one way to reduce your risk of STIs without compromising your pleasure, even if you’re having sex without condoms! There are some limitations to be aware of:
- Gender Identity & How You Have Sex: As of now, research has shown that doxyPEP is safe and effective in cisgender men and transgender women mostly having anal and oral sex. Unfortunately, a recent research study of cisgender women was not able to conclude effectiveness for vaginal sex because a large portion of participants weren’t actually taking their doxyPEP doses. While there is no data yet on doxyPEP for transgender men, those having anal and oral sex should strongly consider it.
- Your HIV Status or PrEP Use: DoxyPEP can be used for people regardless of their HIV status. This means that antibiotics used in doxyPEP do not interact with PrEP medications (that prevent HIV) and HIV treatment (which helps manage your HIV diagnosis).
- Other Health Concerns: If you are allergic to doxycycline, you will not be able to take doxyPEP. Doxycycline use should be avoided if you are pregnant.
What are the side effects?
The most common side effects of doxycycline are sun sensitivity, stomach upset, and irritation of the throat. Not everyone has side effects.
The best way to avoid these side effects is to wear sunscreen, take doxycycline with a full glass of water or other liquid so the pill doesn’t get stuck when you swallow, and don’t lie down for 30 minutes after you take it.
Avoid dairy products, calcium, antacids or multivitamins two hours before or after taking doxycycline.
How can I get my healthcare provider to prescribe doxyPEP?
On June 6th, 2024, the U.S. Centers for Disease Control and Prevention (CDC) published guidelines for healthcare providers about prescribing doxyPEP. Until now, many healthcare providers prescribed it on an “off-label” basis so your healthcare provider might not be aware they can prescribe it for you to prevent STIs.
Here’s some steps you can take to help get on doxyPEP:
- Let your provider know that the CDC updated guidance to make doxyPEP for STI prevention easy to access. Share these guidelines with them or print them out to bring to your appointment.
- If a provider refuses to prescribe it, ask them to document their refusal in your medical chart. If possible, also send a message after your appointment to your provider (either through voicemail or a patient portal) summarizing the visit, including the refusal of prescribing doxyPEP.
- You may need to find a local sexual health clinic at GetTested.CDC.gov who can help you if you have any issues with your typical provider.
Do I still need to get tested for STIs or have any other tests done if I take doxyPEP?
Yes! You should get STI testing (gonorrhea, chlamydia, syphilis) when you start doxyPEP and every 3 months while taking it. If you do not have HIV, you should also be tested for HIV at the same time. Your health care provider might want to check other lab work occasionally to make sure doxyPEP doesn’t affect your liver.
Can I take doxycycline before I have sex to prevent bacterial STIs?
We don’t yet know if taking doxycycline daily has any added benefit for preventing STIs like we do for HIV PrEP. Research studies are currently underway to determine if daily doxyPrEP is effective at preventing bacterial STIs.
*
With DoxyPEP still being relatively new to healthcare providers, you can find support from other community members and activists about their experiences in this Facebook group.