We ♥ PrEP, PEP, & DoxyPEP
HIV medications have been tremendously successful in keeping people living with HIV healthy. They’re also extremely effective at stopping new HIV infections. We are now seeing that antibiotics used to treat STIs are also effective at preventing them before they start. Here’s information about preventing HIV and STIs using medications.
PrEP (for HIV)
What is PrEP?
PrEP stands for Pre-Exposure Prophylaxis. PrEP is an effective way to prevent HIV infection, reducing your chance of getting HIV by up to 99% when taken as prescribed. Currently, there are two methods of PrEP approved by the U.S. Food and Drug administration (FDA):
- Daily oral PrEP pills (one Truvada® or Descovy® pill every day)
- Injectable PrEP (either bi-monthly injectable cabotegravir/Apretude® or twice yearly injectable lenacapavir/Yeztugo®)
Non-daily oral PrEP 2-1-1 with Truvada (also known as “on-demand PrEP”) has also been shown to be effective for certain types of sex (see below for more information). There is no evidence yet whether PrEP 2-1-1 with Descovy is effective.
Who is PrEP for?
PrEP is for HIV-negative people who may be exposed to HIV through sex or injection drug use. According to the U.S. Centers for Disease Control and Prevention (CDC), PrEP should be considered for all adults and adolescents (weighing 77 pounds or more) who are HIV-negative and who sexually-active and/or injecting drugs. This is because anyone of any gender or age can be vulnerable to HIV based on their sex lives or drug use practices.
The CDC recommends PrEP especially for people who’ve had anal or vaginal/front hole sex in the past 6 months AND any of the following:
- A sex partner living with HIV (especially if your partner has an unknown or detectable viral load)
- Bacterial STI–like gonorrhea or chlamydia–in the past 6 months
- Past or current condomless sex with a partner
There are also differences for who can take certain medications for PrEP based on available research data:
- Truvada® (oral pill): Anyone on Truvada can take it daily to prevent HIV transmission during sex and injection drug use. If you are a cisgender man, you may be able to use it on-demand around the time you have sex using PrEP 2-1-1 dosing. (Read more about it below under “What is PrEP 2-1-1?”)
- Descovy® (oral pill): Anyone on Descovy can take it daily to prevent HIV transmission during sex but not for exposure due to injection drug use. While Descovy is approved to reduce the risk of HIV transmission during sex, it is not currently FDA-approved for those who have receptive front hole/vaginal sex.
- Apretude® (injectable long-acting cabotegravir): Long-acting cabotegravir (abbreviated CAB) is approved for use as HIV prevention during sex for people weighing at least 77 pounds, regardless of gender.
- Yeztugo® (long-acting injectable lenacapavir): Lenacapavir (abbreviated LEN) is approved for use as HIV prevention during sex in adults and adolescents weighing at least 77 pounds, regardless of gender.
How do I start and stay on PrEP?
To start oral PrEP (Truvada or Descovy), you will need to:
- See a healthcare provider who will ask you questions, including about your sex life and substance use. If your provider doesn’t ask you about this, it’s best to start the conversation so you can decide which PrEP option is the best HIV prevention choice for you. Your provider will also ask if you have any symptoms of HIV infection.
- Get a blood test for HIV (since you have to be HIV-negative to use PrEP) and hepatitis B & C
- Get a kidney function test (part of your blood test)
- Get a full STI screening (gonorrhea, chlamydia, syphilis)
- Get a lipid panel blood test (only if you’re taking Descovy)
These tests can typically all be done at the same appointment. You may be able to start oral PrEP the same day you have your appointment.
To stay on oral PrEP (Truvada or Descovy), you will need to:
- Get tested for HIV and STIs every three months
- Get a kidney test once a year (if you’re under 50) and every six months (if you’re 50+ years old)
- Get tested for hepatitis C once a year
If you ever stop taking oral PrEP or decide to take PrEP on-demand (PrEP 2-1-1), let your healthcare provider know so you can get the right lab tests done.
To start injectable every two months PrEP (CAB), you will need to:
- See a healthcare provider who will ask you questions, including about your sex life and substance use. If your provider doesn’t ask you about this, it’s best to start the conversation so you can decide which PrEP option is the best HIV prevention choice for you. Your provider will also ask if you have any symptoms of HIV infection.
- Get a blood test for HIV (since you have to be HIV-negative to use PrEP) and hepatitis B & C
- Get a full STI screening (gonorrhea, chlamydia, syphilis)
- Some doctors may start you on a course of daily oral PrEP (typically with oral cabotegravir) called an “oral lead-in.” This makes it easy for people who don’t react well to the drug to stop taking it immediately so that their side-effects go away. If you do not do the “oral lead-in,” some doctors may prescribe a week of oral PrEP to take after you start your CAB injections to allow time for CAB to reach high enough levels in the blood to protect against HIV.
- Receive your first injection. You will get another CAB injection one month later, then switch to every other month injections afterward.
To stay on injectable every two months PrEP (CAB), you will need to:
- Take an HIV blood test at every appointment where you receive your injections.
- Depending on the type of sex you have, you may need to receive STI screenings at your follow up visits.
- Get tested for hepatitis C once per year.
To start injectable twice-yearly PrEP (LEN), you will need to:
- See a healthcare provider who will ask you questions including about your sex life and substance use. If your provider doesn’t ask about this, it’s best to start the conversation so you can decide which PrEP option is the best HIV prevention choice for you. Your provider will also ask if you have any symptoms of HIV infection.
- Get a blood test for HIV (since you have to be HIV-negative to use PrEP) and hepatitis B and C (if recommended).
- Get a full STI screening (gonorrhea, chlamydia, syphilis)
- At your first visit, take two LEN pills.
- At your first visit, you also will receive your first two LEN injections.
- The day after your first visit, you will take two more pills the clinic provided you.
To stay on injectable twice-yearly PrEP (LEN), you will need to:
- Receive two more injections at a clinic every six months.
- Take an HIV blood test at every appointment where you receive your injections.
- You will likely receive STI screenings at your six-month LEN follow-up visits. Your provider may recommend you come in for more frequent STI testing every 3 months (instead of only at your 6 month appointments). At least once per year screening for hepatitis C will also likely be recommended.
If you decide to stop taking injectable PrEP, let your healthcare provider know so that they can help you get the right testing done.
How effective is PrEP?
The simplest answer: very effective. And the more you follow the recommendations, the better it works. Studies show that daily oral PrEP, injectable PrEP, and PrEP 2-1-1 (where you take two pills before sex, then one pill each day for the next 48 hours) are all effective. See your healthcare provider on a regular schedule (often every three to four months) for an evaluation and lab testing, typically including comprehensive STI screening.
There have been very few PrEP failures, in which people have gotten HIV despite following the recommendations. These instances are extremely rare.
Long-acting injectable PrEP may be a more effective HIV prevention option for people who have trouble taking a daily oral pill.
PrEP does not protect people from other sexually transmitted infections (including gonorrhea, chlamydia, syphilis, and herpes).
Health organizations recommend that for the most effective HIV prevention, people who take PrEP combine it with other safe sex strategies, such as using condoms and using your own needles and works when injecting drugs.
How long does it take for PrEP to start working?
It’s important to note that daily oral PrEP doesn’t begin working immediately. When you start taking daily oral PrEP, it takes at least:
- 7 days for the drug to become effective at preventing HIV if you’re having anal sex
- 20 days for the drug to become effective at preventing HIV if you’re having vaginal/front hole sex
If you intend to stop oral PrEP, you should keep on taking it for at least four weeks after you last had sex or injected drugs.
Injectable PrEP has different considerations that pills:
- CAB PrEP will become effective at preventing HIV seven days after the first shot.
- While the exact time to maximum protection against HIV is not known, blood levels of LEN PrEP become high enough within hours after taking the second set of pills. When starting LEN, you should continue using other forms of protection (e.g., condoms) until 2-4 hours after you have taken your second set of oral medications. If you miss the second set of pills, the time to HIV protection increases to 21 days.
- Both LEN and CAB stay in the body a long time after each injection, at decreasing levels over time. You will need to start another PrEP medication six months after your last LEN injection or 8 weeks (2 months) after your last CAB injection if you decide to switch to another form of PrEP.
Side effects of PrEP
There are relatively few side-effects reported by people taking PrEP. These vary by which type or PrEP you use.
If you’re taking oral pills (Truvada or Descovy): Some people report experiencing “start-up syndrome” when they begin PrEP. This can include nausea, headache, loss of appetite, and diarrhea. Usually, symptoms are mild and stop after the first month.
If you have Hepatitis B and stop taking Truvada or Descovy, your Hepatitis B may suddenly get worse. Do not stop taking either medication without first talking to your healthcare provider, as they will need to check your health or give you medicine to treat your Hepatitis B.
Truvada-based PrEP is also associated with small decreases in bone mineral density (bone strength) in some people. People with greater bone density are less likely to suffer from broken bones or fractures after injury, which is why decreases in bone density is important. Decreases in bone strength are usually small, and not associated with fractures or broken bones; bone density increases again after people stop taking Truvada.
Descovy-based PrEP may cause increases in cholesterol and weight.
Oral PrEP, particularly with Truvada, may also affect your kidneys. Following-up with your healthcare provider on a regular schedule is important so that they can perform lab testing to ensure your kidneys are working properly and to determine if you should stop taking PrEP for the time being.
For more information on the differences between Truvada and Descovy, click here.
If you’re taking CAB PrEP (injectable): CAB PrEP’s main side-effects are pain and redness at the injection site. This can occur alongside other possibilities, like diarrhea, headache, and raised liver enzymes. If your doctor is worried about side-effects, you may start on a course of oral cabotegravir for PrEP called an “oral lead-in” before your first injection. This makes it easy for people who don’t react well to the drug to stop taking it immediately so that their side-effects go away.
If you’re taking LEN PrEP (injectable): LEN’s main side effects are injection site reactions, including pain, redness, swelling, itching, and nodules (bumps) under the skin. Use of ice and over-the-counter pain medications may help with these injection site reactions. Headache and nausea are other common side effects with LEN.
What is PrEP 2-1-1?
PrEP 2-1-1 is named for a particular PrEP dosing schedule:
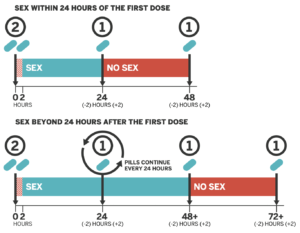
Image: San Francisco AIDS Foundation
- 2 pills are taken 2 to 24 hours before sex
- 1 pill 24 hours after the initial dose
- 1 final pill 24 hours later.
PrEP 2-1-1 is also known as “on-demand,” “event-driven,” “sex-driven” and “intermittent” PrEP.
It is important to know that to date, only oral Truvada has been shown to be effective for PrEP 2-1-1. Studies are currently taking place to determine if Descovy is effective but there is no conclusive data at this point.
How effective is PrEP 2-1-1?
The most well-known study, named IPERGAY, showed that PrEP 2-1-1 reduced risk of HIV infection among cisgender men who have anal sex with cisgender men by 86% compared to placebo. The continuation of the study provided a real-world look at how people use PrEP 2-1-1. This part of the study found that PrEP 2-1-1 reduced risk of HIV infection by 97%. Among those people having sex less frequently, there were zero HIV infections.
It is important to note, however, that PrEP 2-1-1 is neither endorsed by the CDC, nor approved by the FDA, and is considered “off-label” use.
Who might benefit and who should not take PrEP 2-1-1?
PrEP 2-1-1 is only recommended for people having anal sex, since the drug may not be present at levels high enough if using PrEP 2-1-1 to protect vaginal tissues. PrEP 2-1-1 has not been adequately studied in cisgender women, cisgender men who have sex with cisgender women, transgender men, transgender women, people who inject drugs, or people who take Descovy for PrEP or use injectable PrEP. Furthermore, PrEP 2-1-1 is not recommended if you’re living with chronic hepatitis B.
In addition, if you are unable to anticipate when you have sex and cannot take your pre-sex dose of PrEP at least 2 hours (and preferably closer to 24 hours) before sexual activity, 2-1-1 PrEP may not be right for you. If you can’t always plan ahead and take your pre-sex dose at least two hours ahead, or remember to take a second and third dose afterwards, you may instead benefit from daily oral PrEP or injectable PrEP use.
Whatever your decision is about PrEP, or PrEP 2-1-1, be sure to discuss with your healthcare or PrEP provider.
If you switch between 2-1-1 and daily PrEP use, you should retest for HIV prior to restarting if you’ve had sex when you haven’t been taking PrEP.
Where to get PrEP
People can get PrEP in a number of different ways. If you are currently in medical care and have health insurance, you can talk to your regular healthcare provider about PrEP.
You can also look for PrEP-friendly medical providers at PrEPLocator.org (U.S.) or start with our global testing resources to find a clinic who may answer questions about PrEP access in your country.
If you don’t have a medical provider or don’t want to ask them about PrEP, there are additional options for getting PrEP: public sexual health clinics, LGBTQ health centers, local HIV/AIDS service organizations, and in some areas, Planned Parenthood. An easy first step to find PrEP in your area might be to do an internet search for “HIV PrEP (your city or town).”
Some providers may not offer injectable PrEP (CAB or LEN) yet. If your provider doesn’t offer injectable PrEP and you want to learn more, ask if they can refer you to another organization. Depending on your insurance status, you may need assistance from your provider or a PrEP navigator to help you with access to your preferred form of PrEP. Ask your provider or the above-mentioned organizations if they offer PrEP navigation assistance.
How to afford PrEP
PrEP medications can cost thousands of dollars every year, but there are ways to get PrEP at no or low cost.
If you have health insurance, you can expect to pay the normal co-pay for a brand-name drug for oral or injectable PrEP. This cost varies from plan to plan. The manufacturers of all PrEP drugs offer co-pay assistance (see links to Gilead Advancing HIV Access and ViiV Connect). Many Medicare and Medicaid plans also cover PrEP medications. Check with your plan to find out your coverage.
For people without health insurance, including those with certain limited plans that do not include prescription medication coverage, the manufacturers of both oral and injectable PrEP have patient assistance programs. Basic eligibility requirements are that you live in the U.S. and earn equal to or less than 5 times the Federal Poverty Level. For Truvada®, Descovy®, and Yeztugo® (LEN) visit Gilead Advancing Access for more information. For Apretude® (CAB-LA) visit ViiV Connect.
Brand-name PrEP medications are expensive and paying out-of-pocket is impossible for most people. As another option, there are many generic forms of Truvada® (TDF-FTC), some of which cost as little as $30/month. Be sure to ask your provider or PrEP navigator for guidance about paying for PrEP.
A number of U.S. states have established their own PrEP Assistance Programs. Most cover out-of-pocket expenses for the medication for insured patients and almost all programs cover the cost of clinical visits and lab tests regardless of health insurance coverage.
Another option is to participate in a clinical research study or demonstration project of PrEP. You can search for PrEP studies that are now enrolling across the U.S. on the AVAC website.
Resources
Want to learn more about PrEP? Check out these short videos and other resources. You’ll get a quick overview of what PrEP is, how well it works, and how to figure out if it may be right for you.
About PrEP
- PrEP Info (CDC)
- Is PrEP Right for Me? (Greater Than AIDS)
- BHOC Gay Men’s Sexual Health Partnership With Daddyhunt includes PrEP PSAs
- PrEP Medication Guide (CDC)
- What to Know About Truvada (HIV.gov)
- What to know about Descovy (HIV.gov)
- What to know about Cabotegravir (HIV.gov)
- What to know about Lenacapavir (HIV.gov)
Paying for PrEP
- PrEP Medical Assistance Program (Gilead Sciences)
- PrEP Assistance Program for Injectable PrEP (ViiV)
- State PrEP Financial Assistance Programs (NASTAD)
For Your Healthcare Provider
- PrEPLocator.org
- Resources for Consumers and Providers (CDC)
- Prescribing twice yearly LEN PrEP: Clinical Guidelines (New York State Department of Health)
This resource was last updated October 22, 2025.
PEP (for HIV)
You can prevent HIV by taking medications called Post-Exposure Prophylaxis (PEP). PEP must be started within 72 hours (3 days) of when you were potentially exposed (like having condomless sex or sharing syringes) to prevent infection. Find where to get PEP near you here.
What is PEP?
PEP stands for Post-Exposure Prophylaxis. PEP prevents HIV infection in people who have been recently exposed to HIV. If you are HIV-negative but recently had condomless sex with someone whose HIV status you didn’t know, for example, consider taking PEP to prevent a possible HIV infection. If you have HIV, and think there’s a chance you exposed someone else to HIV, you can tell that person about PEP.
PEP is a four-week course of anti-HIV medications that prevent HIV infection. In order for PEP to work, it has to be started as soon as possible after the HIV exposure event.
That means if you think you’ve been exposed to HIV, and want to start taking PEP, do so as soon as possible. PEP has to be started within 72 hours (3 days) in order to work.
Should I go on PEP?
If you’re HIV-negative, not on PrEP, and your answer to any of the questions below is yes, talk to your doctor right away.
- Did you bottom without a condom with someone who is either HIV-positive and not undetectable or someone whose HIV status you don’t know?
- Did the condom break and you got a load up your butt?
- Did you top someone without a condom who is either HIV-positive and not undetectable or someone whose HIV status you don’t know?
- Have you shared needles with someone?
What is PEP for?
PEP is for HIV-negative people who may have been exposed to HIV during a single event. PEP is not a substitute for other proven HIV prevention methods, such as correct and consistent condom use, PrEP (pre-exposure prophylaxis), or use of sterile injection equipment.
How does PEP work?
You have to start PEP within 72 hours of exposure for PEP to work. Seek PEP right away if you think you’ve been exposed to HIV and you are not on PrEP. Your doctor will determine what treatment is right for you based on how you may have been exposed to HIV.
PEP consists of three antiretroviral medications that are taken for 28 days. PEP is safe but may cause side effects like nausea in some people. These side effects can be treated and are not life threatening. PEP is not 100% effective; it does not guarantee that someone exposed to HIV will not become infected with HIV.
What happens after I start PEP?
Make sure you take your meds. PEP does not work if you do not take the medications.
Continue to use condoms with sex partners while taking PEP and do not use injection equipment that has been used by others. This will help avoid spreading the virus to others if you become infected.
Return to your healthcare provider for more HIV testing one month, three months, and six months after the potential exposure to HIV. Your healthcare provider will give you a follow-up schedule.
Adapted from SFAF
DoxyPEP (for Chlamydia, Syphilis, & Gonorrhea)
Find doxyPEP here.
What is doxyPEP?
DoxyPEP stands for doxycycline post-exposure prophylaxis, a new way to decrease the chance of getting a bacterial sexually transmitted infection (STI).
Doxy is shorthand for doxycycline, a common antibiotic used to treat bacterial infections. You may have taken it for a skin condition or after you got diagnosed with a bacterial STI in the past.
Post-exposure prophylaxis means that a person receives treatment after an exposure. With doxyPEP, someone can take doxycycline following oral, anal, and vaginal/front hole sex.
The difference between doxyPEP and getting treated for an STI comes down to two main things:
- You’re taking treatment medications before you have symptoms
- You’re taking treatment medications before you test positive for an STI
Which STIs does doxyPEP prevent?
DoxyPEP has been shown to prevent three major STIs: chlamydia, syphilis, and sometimes gonorrhea in cisgender men and transgender women, mostly having anal and oral sex.
While doxyPEP does not prevent HIV, there are two options for people who want to reduce their HIV risk: HIV PrEP (taken before sex or potential exposure to HIV) or HIV PEP (taken after potential exposure to HIV).
Using condoms & lube are still an effective way to reduce your chance of getting HIV and other STIs. Find out how to prevent other STIs here.
How do I use doxyPEP?
A person takes 200mg of doxycycline up to 72 hours after they have oral, anal, or vaginal/front hole sex. It’s better to take it within 24 hours after sex, but you can take it up to 72 hours after. Doxycycline is safe to take daily if you’re having frequent sex.
Remember, the current guidance for doxyPEP is to take medications after sex, not used before sex like PrEP for HIV. We don’t yet know if taking doxycycline daily or before sex has any added benefit for preventing STIs like we do for HIV PrEP. Research studies are currently underway to determine if daily DoxyPrEP is effective at preventing bacterial STIs.
How effective is it?
A research study that enrolled cisgender men who have sex with men and transgender women in San Francisco and Seattle showed that doxyPEP decreased the risk of bacterial STIs by an average of 65% (with 74-88% reduction for chlamydia and syphilis, and 55-57% reductions in gonorrhea). However, the efficacy of doxyPEP in this study by the STI and the HIV status of participants.
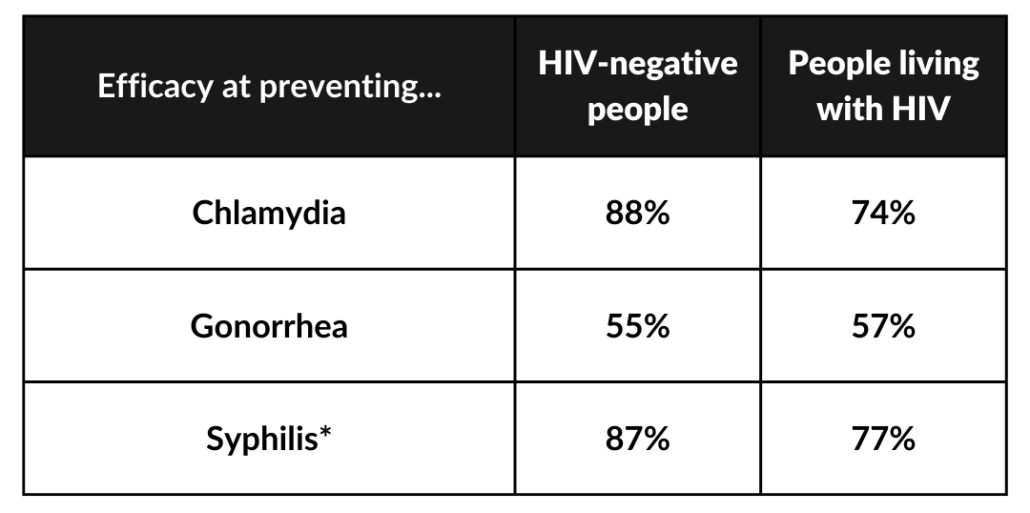
*In the studies, the number of syphilis infections was so small they couldn’t make broad statements about its efficacy for everyone.
Who can use doxyPEP?
If you are a cisgender man or transgender woman, doxyPEP is one way to reduce your risk of STIs without compromising your pleasure, even if you’re having sex without condoms! There are some limitations to be aware of:
- Gender Identity & How You Have Sex: As of now, research has shown that doxyPEP is safe and effective in cisgender men and transgender women mostly having anal and oral sex. Unfortunately, a recent research study of cisgender women was not able to conclude effectiveness for vaginal sex because a large portion of participants weren’t actually taking their doxyPEP doses. While there is no data yet on doxyPEP for transgender men, those having anal and oral sex should strongly consider it.
- Your HIV Status or PrEP Use: DoxyPEP can be used for people regardless of their HIV status. This means that antibiotics used in doxyPEP do not interact with PrEP medications (that prevent HIV) and HIV treatment (which helps manage your HIV diagnosis).
- Other Health Concerns: If you are allergic to doxycycline, you will not be able to take doxyPEP. Doxycycline use should be avoided if you are pregnant.
What are the side effects?
The most common side effects of doxycycline are sun sensitivity, stomach upset, and irritation of the throat. Not everyone has side effects.
The best way to avoid these side effects is to wear sunscreen, take doxycycline with a full glass of water or other liquid so the pill doesn’t get stuck when you swallow, and don’t lie down for 30 minutes after you take it.
Avoid dairy products, calcium, antacids or multivitamins two hours before or after taking doxycycline.
How can I get my healthcare provider to prescribe doxyPEP?
On June 6th, 2024, the U.S. Centers for Disease Control and Prevention (CDC) published guidelines for healthcare providers about prescribing doxyPEP. Until now, many healthcare providers prescribed it on an “off-label” basis so your healthcare provider might not be aware they can prescribe it for you to prevent STIs.
Here’s some steps you can take to help get on doxyPEP:
- Let your provider know that the CDC updated guidance to make doxyPEP for STI prevention easy to access. Share these guidelines with them or print them out to bring to your appointment.
- If a provider refuses to prescribe it, ask them to document their refusal in your medical chart. If possible, also send a message after your appointment to your provider (either through voicemail or a patient portal) summarizing the visit, including the refusal of prescribing doxyPEP.
- You may need to find a local sexual health clinic at GetTested.CDC.gov who can help you if you have any issues with your typical provider.
Do I still need to get tested for STIs or have any other tests done if I take doxyPEP?
Yes! You should get STI testing (gonorrhea, chlamydia, syphilis) when you start doxyPEP and every 3 months while taking it. If you do not have HIV, you should also be tested for HIV at the same time. Your health care provider might want to check other lab work occasionally to make sure doxyPEP doesn’t affect your liver.
Can I take doxycycline before I have sex to prevent bacterial STIs?
We don’t yet know if taking doxycycline daily has any added benefit for preventing STIs like we do for HIV PrEP. Research studies are currently underway to determine if daily doxyPrEP is effective at preventing bacterial STIs.
*
With DoxyPEP still being relatively new to healthcare providers, you can find support from other community members and activists about their experiences in this Facebook group.