STIs (Sexually Transmitted Infections)
The most important thing to know about STIs: get tested every three to six months. Get a blood test and pee in a cup. If you’re giving oral sex (blowjobs or eating out) or having anal sex, ask your doctor to swab your mouth and butt as well!
Many STIs don’t cause symptoms. But if you have burning or discharge from your penis, vagina/front hole, throat or butt, discomfort when you pee, a rash and/or ulcer in your mouth or on your genitals, don’t wait: go get that test! To find a free or low-cost test near you, go to gettested.cdc.gov.
Most STIs can be cured, and getting early treatment is the best way to do so.
Condoms are also effective at preventing STIs, and some STIs can now be prevented with medications using a strategy called doxyPEP.
Tell a partner about your positive result
One of the most important things you can do if you get diagnosed with an STD is to tell your partners. That way, they can get tested too.
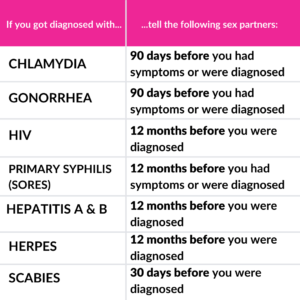
Adapted from TellYourPartner.org
Look at this chart to see how far back you have to go when thinking about who you need to tell.
Depending on how well you know the person – or persons – you have sex with, or agreements you have – it may not be a big deal to tell them you may have unintentionally exposed them to an STD. In other situations, it can be hard. You might feel awkward, scared, and worried about your partner’s reaction. Your local health department can also help, and will protect your anonymity too.
For tips on how to tell them yourself, here are some suggestions.
Telling your partners is good for your partner’s health and your own. It also feels good to know you’ve let them know.
Syphilis
The number of people who are getting syphilis is increasing, especially among gay and bi cis men. Syphilis is easily transmitted between sex partners since symptoms are not always visible and symptoms go away even when not treated. If you’re having sex, get tested for syphilis every three months.
What is syphilis?
Syphilis is a blood infection caused by the bacteria Treponema pallidum.
How do you get syphilis?
You can get syphilis by touching a sore caused by syphilis—called a lesion or chancre—on another person. People who have syphilis usually get lesions on their genitals or butt or inside their rectum or vagina/front hole. People can also get lesions on their lips or in their mouth which may be infectious.
What are the symptoms of syphilis infection?
Many times, people with syphilis don’t know they have it because they don’t get any symptoms. When people do experience symptoms, they usually appear in three stages.
Stage 1:
Within a few weeks after you’ve been infected on the part of your body where you were infected (usually on your penis, balls, mouth, throat, rectum or in your butt or vagina/front hole), you’ll get a sore. It might be painful, but usually it isn’t. It’s also often hard to see. It will scab over, then heal. Even without treatment, it will go away on its own but the infection will progress to the next stage.
Stage 2:
Two to six weeks after Stage 1 infection, you might get a rash. This rash could be on your chest, back, palms of your hands, the soles of your feet, scrotum, vulva, or other parts of your body. You also might get a fever, have a sore throat, lose your hair in patches, have headaches, have swollen lymph glands, lose weight, be tired or have muscle and joint aches. These symptoms can come and go for weeks to months and, without treatment, the infection will progress to the next stage.
Other medications may be used if a person with syphilis is allergic to penicillin.
Stage 3:
Without treatment, a syphilis infection will begin to damage your internal organs and other parts of your body–such as your brain, nerves, eyes, heart, blood vessels, liver, bones, and joints. This kind of damage might not be noticeable for years, and in very rare cases might be serious enough to cause death.
Even when a person with syphilis doesn’t show any symptoms, they are still able to transmit syphilis to others.
Testing
Syphilis is diagnosed with a blood test. If you’re having sex, get tested for syphilis, HIV, gonorrhea and chlamydia every three months. For more testing information, you can find free and low-cost testing for both STDs and HIV at gettested.cdc.gov.
Testing for syphilis typically requires a combination of tests to determine if you have an active infection. One test is an enzyme immunoassay (EIA) which detects syphilis antibodies. Another test is an RPR, which detects active infection. There may be other tests your healthcare provider will use to identify a current syphilis infection.
If you’ve ever had syphilis in the past, the EIA test will be will always be reactive (aka positive). Make sure to tell your health care provider about that past infection so that you can get an RPR (since the EIA will always be reactive). The RPR is used to determine if someone with a history of syphilis has been re-infected.
Can syphilis be treated?
Syphilis can be treated with penicillin, and cured if diagnosed early on. Other drugs are used if a person with syphilis is allergic to penicillin.
How can it be prevented?
Don’t touch another person’s syphilis sores or lesions. Condoms, dental dams, or gloves that cover sores will help prevent infection. DoxyPEP can be about 70% effective in reducing your chance of getting syphilis, even after condomless sex.
If you’re on treatment for syphilis, wait to have sex with other people until your sores are completely healed.
Resources:
Gonorrhea
How do you get gonorrhea?
Gonorrhea can be spread during anal, oral and vaginal/front hole sex.
What are the symptoms of gonorrhea infection?
Symptoms may be different or even non-existent, depending on your body. It’s pretty common for a person with a penis to have gonorrhea but not to have any symptoms, and even more so if the infection is in their butt or throat. For people with vaginas/front holes, pain/burning when urinating, discharge, and/or bleeding between periods are common. If you have gonorrhea you might get symptoms like a dry or sore throat, itchiness and pain when you have a bowel movement, a discharge from your penis or vagina/front hole, and/or pain or burning when you pee. An infection in your throat might cause discharge, but this is less common. Symptoms can take between two and ten days to show up. Rarely, if left untreated, gonorrhea can get into your blood and cause joint pain, rashes, or other symptoms.
What is disseminated gonorrhea?
Without treatment, gonorrhea of the penis, throat, rectum, or vagina/front hole can spread throughout the body, causing something called disseminated gonorrhea (also known as DGI). DGI can cause joint pains, redness, or swelling as well as fevers and/or a rash of red or pink spots that may become filled with clear fluid or pus. DGI can also cause serious infections of the blood, heart valves, or nervous system (including meningitis). In rare cases, people may die from DGI. DGI is treated differently from gonorrhea of the penis, throat, rectum, or vagina/front hole. It requires multiple days or even weeks of antibiotics, usually given through the veins. DGI not very common but it is on the rise in some parts of the country. Contact your healthcare provider if you have DGI symptoms. The only way to prevent DGI is to get tested and treated for gonorrhea.
Testing
You’ll probably know if you have an infection in your penis or vagina/front hole. But just in case, make sure to tell your healthcare provider if you are experiencing any of the symptoms above or if one of your partners was recently diagnosed with an STD. For more testing information, you can find free and low-cost testing for both STDs and HIV at GetTested.CDC.gov.
Can gonorrhea be treated?
We can cure a gonorrhea infection with antibiotics. But you shouldn’t have any sex for seven days after you start your antibiotics to make sure the infection goes away. Gonorrhea is also a smart bacterium, and has developed resistance to several kinds of antibiotics. CDC now recommends taking a shot of ceftriaxone to treat gonorrhea of the penis, throat, rectum, or vagina/front hole. If your symptoms continue for more than a few days after you get treated, you should go back to your healthcare provider and get checked.
How can it be prevented?
Using a condom when you have sex can help prevent you from getting gonorrhea, if the area that’s infected (e.g., your partner’s penis, vagina/front hole, throat or butt) is covered. While doxyPEP can be used to prevent gonorrhea, it is not very effective for this particular STI. Sex toys can also spread gonorrhea if shared between partners, so make sure to cover toys with a condom and wash them after use.
Resources:
Chlamydia
Chlamydia is one of the most common STDs in the U.S., with over a million new cases reported every year.
What is chlamydia?
Chlamydia is a bacterial infection that can happen in your urethra (where you pee from), rectum (butt), vagina (front hole) or throat. It’s caused by the bacteria Chlamydia trachomatis.
How do you get chlamydia?
Chlamydia can be spread during anal, oral and vaginal sex.
What are the symptoms of chlamydia infection?
Most people will have no symptoms, especially if the site of infection is the butt or throat. Symptoms may not show up for a week, but you can still be infectious during that time.
Symptoms can cause itchiness and pain when you poop, or abnormal discharge from your vagina/front hole or penis and pain when you pee. A dry or sore throat can also occur, but this is uncommon.
Testing
A medical practitioner can diagnose chlamydia by swabbing your throat, vagina/front hole, or butt. Urine tests are usually used to test for chlamydia infection in the urethra. For more testing information, you can find free and low-cost testing for both STDs and HIV at GetTested.CDC.gov.
How is chlamydia treated?
We can cure a chlamydia infection with antibiotics. If you had sex while you were infected with chlamydia, your sexual partners should also get tested for chlamydia and treated if they are infected. But you shouldn’t have any sex for seven days after you start your antibiotics to make sure the infection goes away.
How can it be prevented?
You can lower the risk of getting chlamydia by using condoms and testing frequently. DoxyPEP can also reduce your chance of chlamydia by up to 88%, even after having condomless sex.
Resources
Hepatitis A
What is it?
Hepatitis A is a very contagious liver infection caused by the hepatitis A virus.
How do you get it?
Most often, people get hepatitis A when they come into contact with fecal matter from someone with hepatitis A. This might happen during activities like ass play and rimming, or by touching an infected person’s butt during sex and then not washing your hands before eating or drinking.
“Hepatitis A can be spread from close, personal contact with an infected person, such as through certain types of sexual contact (like oral-anal sex), caring for someone who is ill, or using drugs with others. Hepatitis A is very contagious, and people can even spread the virus before they feel sick.”
The virus can also be transmitted in water (e.g., by eating shellfish from contaminated water sources) or orally (e.g., by sharing eating utensils, sharing a joint, or by kissing an infected person).
What are the symptoms?
People with hepatitis A might get mild flu-like symptoms, nausea and vomiting, abdominal pain, joint and muscle pain, and jaundice (yellowing of the skin, eyes or urine). Symptoms may take between two and seven weeks to show up but the infection usually clears the body within a month. Rarely, people can be sick for several months.
Testing
A blood test is used to diagnose hepatitis A. Once you have had hepatitis A, you’ll have antibodies in your blood and will probably become immune to it. That means once you’ve had it, you probably won’t get it again. For more testing information, you can find free and low-cost testing for both STDs and HIV at GetTested.CDC.gov.
Can it be treated?
There are no specific treatments for hepatitis A after a person has become infected. Some people need to go to the hospital for things like fluids and close monitoring. This illness can be prevented by getting the hepatitis A vaccine.
How can it be prevented?
The CDC recommends that all gay and bi cis men and trans people get a hepatitis A vaccine. The vaccination comes in two required doses—the second dose is given six months after the first. There is also a hepatitis A and B combined vaccination that’s available, which comes in three doses. The second dose is given one month after the first; the third six months after the initial dose.
To prevent hepatitis A transmission, wash your hands after using the bathroom and before and after sex (especially ass play), and use dental dams for rimming.
Hepatitis A & HIV
There is a higher risk for severe hepatitis A amongst people who have HIV. It is recommended to get a hepatitis A vaccine if you have HIV.
Resources:
Hepatitis B
What is hepatitis B?
Hepatitis B is a liver infection caused by the hepatitis B virus. The virus causes liver inflammation and can lead to liver disease.
How do you get hepatitis B?
You can get hepatitis B if the blood, semen, saliva or other body fluid from a person with hepatitis B enters your body. That means you can get hepatitis B from an infected person during condomless oral or anal sex, or by using an infected person’s toothbrush, razor or injection equipment.
What are the symptoms of hepatitis B infection?
People who have hepatitis B infection may experience mild flu-like symptoms, nausea and vomiting, abdominal pain, joint and muscle pain and jaundice (yellowing of the skin, eyes or urine). Symptoms may take between one and six months to appear. Some people do not get any symptoms.
Most adults will recover completely from hepatitis B without treatment. But some people may develop a chronic hepatitis B infection, which lasts for more than 6 months. People who develop a chronic hepatitis B infection may be at risk of developing cirrhosis and liver cancer.
Testing
A blood test is used to diagnose hepatitis B. People who have had hepatitis B once already probably won’t get it again. This is because they developed antibodies to it when they first were infected and now they are immune to the infection. For people who don’t naturally recover from hepatitis B on their own, the infection should be monitored with blood tests, called liver function tests, for the rest of their lives. For more testing information, you can find free and low-cost testing for both STDs and HIV at GetTested.CDC.gov.
Can hepatitis B be treated?
There is no cure for hepatitis B, but most people who were infected as adults clear the infection from their body on their own. People who do develop chronic hepatitis B should speak to their regular doctor about treatment options. People with liver damage may need to be treated while people without liver damage may not need treatment.
The treatment options won’t cure hepatitis B, but they can decrease the severity of the infection and prevent liver damage as well as reduce the risk of transmitting it to someone else. Sometimes, people are prescribed antiviral medications, like Truvada, which can be used to treat hepatitis B.
How can hepatitis B be prevented?
The CDC recommends that all gay and bi cis men and trans people should be tested for hepatitis B and if not infected or immune, vaccinated. The vaccination is delivered in a series of three doses. After the first dose, the second and third doses are delivered at 1 and 6 months, respectively.
There’s also a combination hepatitis A and B vaccination (see hepatitis A page for details).
To reduce the risk of getting or giving Hepatitis B:
- Use condoms during sex (and put on a new one between partners);
- Use gloves and lube during fisting (change between partners);
- Don’t share sex toys (or put condoms on insertive toys and change them between partners);
- Wash your hands and sex toys after sex and between partners;
- Don’t share injection equipment such as needles, syringes, swabs, spoons, filters, water and tourniquets. Use new equipment, and wash your hands before and after injecting;
- Don’t share toothbrushes, razors, nail clippers, or nail scissors;
- Make sure body artists use sterile equipment for tattoos, piercings, and other body art; and,
- Wear disposable gloves if you give someone first aid or are cleaning up blood or other body fluids.
Hepatitis B & HIV
People with HIV that get hepatitis B might have to temporarily stop taking their antiretroviral HIV medications and medications they may take for opportunistic infections. This is because many HIV medications are processed by the liver, and can’t be tolerated during acute hepatitis B illness.
People with HIV who get hepatitis B may experience a more rapid progression of their HIV illness, although studies have not established this entirely.
Resources:
Hepatitis C
What is hepatitis C?
Hepatitis C is a liver infection caused by the hepatitis C virus (HCV). Infection with the virus causes liver inflammation and can cause liver disease.
How do you get hepatitis C?
Hepatitis C is transmitted from contact with infected blood. You can get infected if even a small amount of infected blood gets into your bloodstream. Sharing needles, syringes, or other equipment to inject drugs can transmit hepatitis C. People also get hepatitis C from needle sticks and sharps injuries in healthcare settings.
It’s also possible to transmit hepatitis C by sharing toothbrushes, razors, or tattoo and piercing equipment.
People living with HIV are getting hepatitis C more and more, even though historically, sexual activity was thought of as a low-risk activity for transmission. Some of these cases might be from sharing injection equipment, but it seems that most are due to sexual transmission.
Hepatitis C transmitted during sex usually happens during condomless anal sex. Risk of transmission goes up with any sexual activity that damages the lining of the anus—such as fisting, sex sessions that last a long time or rough sex. Group sex, party drug use before sex and using unwashed sex toys can also put you at risk of hepatitis C if you’re exposed to blood or you have breaks in your skin.
The hepatitis C virus also lives in semen, but whether or not this adds to the risk of transmitting hepatitis C during condomless anal sex is unknown.
What are the symptoms or signs of hepatitis C infection?
A lot of people with hepatitis C won’t experience any symptoms. Other people may get flu-like symptoms, nausea, or abdominal pain pretty soon after getting infected. During the first 2 to 6 months after getting infected, about one in four people clear the virus from their body on their own. Others go on to develop a chronic hepatitis C infection, which can result in cirrhosis and liver cancer after many years.
How do I get tested for hepatitis C?
A combination of blood tests is used to diagnose hepatitis C. If you’re living with HIV, you may need to be tested for hepatitis C once a year. Testing more frequently may be recommended for HIV-positive individuals who are sharing drug equipment, have sexual activity that might case trauma or breaks in tissue, or having sex without condoms.
If you have hepatitis C now or have had it in the past, you have hepatitis C antibodies in your blood. But even if your body clears the infection on its own, you could get re-infected if you come into contact with the virus again. You don’t develop immunity to the hepatitis C virus (unlike hepatitis A and hepatitis B).
For people who don’t clear the virus on their own, the infection will be monitored with liver function tests.
For more testing information, you can find free and low-cost testing for both STDs and HIV at gettested.cdc.gov.
Can hepatitis C be treated?
There are newer treatments now available for hepatitis C that can clear the virus from your body and prevent the virus from causing cirrhosis (scarring) of the liver, liver cancer or liver failure. These new treatments are highly effective, with limited side-effects, even for people who are infected with HIV. Most people can be cured in 8 to 12 weeks.
Some people find complementary therapies and lifestyle changes to be helpful in managing hepatitis C symptoms.
Treatment options for people who are coinfected with HIV and hepatitis C can be more complicated. Your doctor will be able to tell you more about your treatment options. Talk to your doctor about your treatment options.
How can hepatitis C be prevented?
There isn’t a vaccine you can get to prevent hepatitis C infection.
Here’s what you can do to reduce the likelihood that you’ll get hepatitis C:
- Don’t share injection equipment like needles, syringes, swabs, spoons, filters, water or tourniquets. Always use new injection equipment;
- Use condoms and water- or silicon-based lube during anal sex, especially if there is blood or other STIs
- Wear gloves and use water- or silicon-based lube during fisting
- Don’t share sex toys with sex partners. Or, put a condom over insertive sex toys and change them between different partners
- Don’t share personal items like toothbrushes, razors, nail clippers, or nail scissors
- Make sure body artists use new and sterile equipment if you get tattoos, body piercings or other body art
- Wear disposable gloves if you give someone first aid or are cleaning up blood or other body fluids
Hepatitis C & HIV co-infection
People living with HIV are more likely to have hepatitis C than people who are HIV-negative. This might be because behaviors that expose a person to HIV might also expose them to hepatitis C.
A person co-infected with hepatitis C and HIV:
- May have more difficulty getting an accurate hepatitis C test result (i.e., may be more likely to get a false-negative or indeterminate test reading);
- May have a higher concentration of the hepatitis C virus in their body fluids;
- May have higher HIV viral loads but probably won’t experience faster HIV disease progression;
- Can safely treat both infections. People with both infections should have their liver enzymes monitored regularly since HIV medications can cause liver inflammation or damage.
Resources
Shigella
Shigella is a bacteria that can be spread through oral-anal contact. Shigella causes an infection called shigellosis, which can cause diarrhea, fever, and stomach cramps,
Practicing good hygiene is a good way to prevent shigellosis. Wash your hands and genitals thoroughly after using the bathroom. Using a dental dam when rimming can reduce risk. Showering and douching can also decrease the chance of infection before rimming. If you have condomless anal sex, the top (or insertive partner) should wash their penis before being sucked.
Shigella infections may resolve on their own in 5 to 7 days in people with healthy immune systems. Other people may need to be treated with antibiotics.
For more testing information, you can find free and low-cost testing for both STIs and HIV at GetTested.CDC.gov.
Resources
Herpes
Herpes can be caused by two different herpes simplex viruses (HSV type I and type II). You can give or get herpes whenever there is direct skin-to-skin contact and during oral, anal, or vaginal sex. Transmission can occur from many forms of intimate contact. These can include kissing, blow jobs, rimming, and fisting. Condoms can help prevent herpes transmission, but they aren’t 100% effective.
Most oral herpes cases, with fever blisters and cold sores on the mouth, are caused by HSV type I. Most genital herpes cases, with sores on the vagina, penis or anus—or the skin around those areas—are caused by HSV type II. Since many people have oral sex, type I is increasingly causing genital herpes cases. Once you are infected with HSV, it will live in your body forever. It may cause symptoms occasionally or may not cause any symptoms at all.
To accurately diagnose herpes, laboratory tests are recommended.
For more testing information, you can find free and low-cost testing for both STIs and HIV at GetTested.CDC.gov.
Resources:
- CDC Fact Sheet
- Something Positive for Positive People
Herpes support group & information - No Shame in This Game
Stories about living with herpes & a documentary video - Herpes 101 Resources
- Herpes Opportunity
Addresses the stigma and shame that comes with a herpes diagnosis
Provides herpes disclosure fact sheets
Crabs & Scabies
Crabs
Pubic lice – also known as crabs, since that’s what they look like – live on pubic and other body hair (but not head hair). They can be spread without sexual contact, for instance by sharing bath towels or clothing. You might have pubic lice if you have itching where your pubic hair is, your skin in that area is irritated, or if you see specks of blood on your skin there.
The treatment for pubic lice is a topical medicated lotion that can be bought without a prescription. Following treatment, most nits will still be attached to hair shafts. Nits may be removed with fingernails or by using a fine-toothed comb.
- To kill any lice or nits remaining on clothing, towels, or bedding, machine-wash and machine-dry those items that the infested person used during the 2–3 days before treatment. Use hot water (at least 130°F) and the hot dryer cycle.
- Items that cannot be laundered can be dry-cleaned or stored in a sealed plastic bag for 2 weeks.
Resources
Scabies
Scabies are tiny mites – smaller than crabs – that can burrow into the skin. They can cause intense itching and a pimple-like skin rash, although the first time someone gets them, symptoms may not show up for four to eight weeks.
Usually they’re spread by direct, prolonged, skin-to-skin contact with a person who has them. They’re diagnosed often based on the rash and the presence of burrows, although when possible it’s good to get the diagnosis confirmed using a microscope.
Scabies lotions and creams aren’t available over the counter, and you’ll need a doctor’s prescription. Make sure to follow the instructions carefully, Bedding and clothing worn or used next to the skin anytime during the 3 days before treatment should be machine washed and dried using the hot water and hot dryer cycles or be dry-cleaned. Items that cannot be dry-cleaned or laundered can be disinfested by storing in a closed plastic bag for several days to a week.
For more testing information, you can find free and low-cost testing for both STDs and HIV at GetTested.CDC.gov.
Resources
HPV
What is HPV?
There are many types of Human Papillomavirus (HPV). About 40 types of HPV can be transmitted during oral, anal, and vaginal/front hole sex. HPV is very common. If you are having sex, you will likely become infected with HPV at some point in your life. This is true for all genders.
The good news is that, in most cases (9 out of 10), HPV infections will go away on their own within 2 years. You won’t even know it was there. The bad news is, that if it doesn’t, HPV can cause some serious health problems.
- HPV can cause cancer. HPV is the main cause of cervical and anal cancer. It can also cause oral (back of the throat), penile, vaginal, cervical, and vulvar cancers. These cancers can take many years (even decades) to develop after the initial infection.
- HPV can cause warts. HPV can cause warts around the genitals and anus. The warts can be removed, but the underlying HPV infection cannot be treated. That is why warts can keep coming back after they are removed.
How do you get HPV?
HPV is very contagious. You get it through skin-to-skin contact. That means it is not transmitted through body fluids (e.g., semen) and you don’t have to be penetrated to get it. Skin-to-skin friction is all it takes (e.g., grinding, licking, thrusting).
What are the symptoms of HPV infection?
Most people with HPV will not know they have it. In the majority of cases, there are no symptoms. That means it’s easy to spread to your sex partners.
Can you get tested for HPV?
If you have a cervix, you can be screened with a cervical Pap smear for high-risk HPV that can cause cervical cancer. Anal Pap smears are also available for people who have anal sex to see if you have high-risk HPV. There are no other tests to find out a person’s “HPV status.”
How is HPV treated?
Currently we have no treatment for HPV infections. That means even if we treat the disease caused by HPV infection (e.g., warts, cancer), the underlying infection may remain.
How is HPV prevented?
The most effective prevention for HPV is vaccination. The HPV vaccine is proven safe and effective at preventing HPV transmission of 9 HPV types. These types cause the majority of genital warts and cancer. It is recommended that everyone between the ages of 9 and 26 be vaccinated. Adults aged 27 to 45 can still be vaccinated, but they should discuss this with their healthcare provider because the vaccine may be less effective for older adults.
Can condoms prevent HPV?
Condoms can help reduce the risk of HPV transmission, but remember HPV is spread from skin-to-skin contact. That means HPV can be transmitted from areas of the skin where a condom doesn’t cover.
Resources
Bacterial Meningitis
Bacterial Meningitis is a severe bacterial infection that causes inflammation of the membranes covering the brain and spinal cord. It can be serious and is sometimes fatal. People living with HIV are at a greater risk than the general population of getting meningitis.
It’s spread through the exchange of respiratory and throat secretions such as saliva. You can get it from someone who is infected by kissing, oral or anal sex, or sharing cigarettes or smoking equipment such as pipes or bongs.
There is an effective vaccine. One shot is given for people who are HIV-negative and two shots for people who are living with HIV. There are treatments for meningitis but it’s important to get treatment right away.
For more testing information, you can find free and low-cost testing for both STIs and HIV at GetTested.CDC.gov.
Resources:
- Fact Sheet from the Meningitis Foundation
- CDC Fact Sheet
Mycoplasma genitalium (Mgen)
What is Mycoplasma genitalium?
Mycoplasma genitalium (Mgen) is a bacterial infection that can occur in your urethra (where you pee from). It accounts for about 15-20% of STIs found in the urethra that are otherwise not due to gonorrhea. Its role as a cause of infection in the throat, vagina/front hole, or butt is still unclear.
How do you get Mycoplasma genitalium?
Mycoplasma genitalium can be spread during sexual activity, including anal or vaginal/front hole sex.
What are the symptoms of Mycoplasma genitalium?
The typical symptoms include those of ‘urethritis’, which are pain with urination, itching and/or discharge. However, many cases are asymptomatic.
Should you get tested?
Routine screening for Mycoplasma genitalium is not currently recommended. If you have persistent or recurrent urethritis (infection of your urethra) discuss Mycoplasma genitalium with your healthcare provider.
Can Mycoplasma genitalium be treated?
Mycoplasma genitalium infection can be cured with antibiotics.
How can it be prevented?
You can lower the risk of getting Mycoplasma genitalium by using condoms during sex.
Resources
Get your vaccines
Mpox virus continues to circulate in 2025. Here’s what you need to know.
In addition to routine adult immunizations, gay, bi, queer, and trans people should make sure they get these vaccines:
Hepatitis A
What is hepatitis A?
Hepatitis A is a serious liver disease.
How is it spread?
It can be spread from person to person through contact with the feces (stool) of people who are infected. This can happen during mouth-to-anus contact (rimming) or from contaminated food, water, or objects.
What are symptoms of hepatitis A?
Symptoms of hepatitis A can include:
- Fever, tiredness, loss of appetite, nausea and vomiting
- Severe stomach pains and diarrhea
- Jaundice (yellow skin or eyes, dark urine, clay-colored bowel movements)
These symptoms usually appear 2-6 weeks after exposure and typically last less than 2 months, although some people can be ill for as long as 6 months.
The hepatitis A vaccine
You will need two doses for long-lasting protection. These doses should be given at least six months apart.
Resources
Hepatitis B
What is hepatitis B?
Hepatitis B is a serious liver disease. It can be described as “acute”, lasting a few weeks or “chronic”, leading to a serious, lifelong illness.
How is it spread?
It can be spread when blood, semen, or other body fluid infected with the hepatitis B virus enters the body of a person who is not infected.
What are symptoms of hepatitis B?
Hepatitis B can be either acute or chronic.
Acute hepatitis B virus infection is a short-term illness that occurs within the first 6 months after someone is exposed to the hepatitis B virus. This can lead to:
- Fever, tiredness, loss of appetite, nausea and/or vomiting
- Jaundice (yellow skin or eyes, dark urine, clay-colored bowel movements)
- Pain in muscles, joints, and stomach
Chronic hepatitis B virus infection is a long-term illness that occurs when the hepatitis B virus remains in a person’s body. Most people who go on to develop chronic hepatitis B do not have symptoms, but it is still very serious and can lead to:
- Liver damage (cirrhosis)
- Liver cancer
- Death
Chronically infected people can spread hepatitis B virus to others, even if they do not feel sick themselves.
The hepatitis B vaccine
You will typically need 2-3 doses for long-lasting protection, depending on which type of hepatitis B vaccination you receive. The three dose-vaccine series should be given over a period of 6 months.
Resources
______________________________________________________________________________________
HPV
What is HPV?
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States. CDC estimates that there were 43 million HPV infections in 2018. HPV is so common that almost every person who is sexually-active will get HPV at some time in their life if they don’t get the HPV vaccine. Health problems related to HPV include genital warts and cervical cancer.
How is it spread?
It can be spread through skin-to-skin contact, usually during oral, vaginal/front hole, or anal sex with someone who has the virus. Most people will become infected at some point in their lives. The majority of infections will go away on their own and not cause serious problems.
What are symptoms of HPV?
In most cases, HPV goes away on its own and does not cause any health problems. But when it does not go away, it can cause health problems like genital warts and cancer (oral, anal, cervical, and penile cancer). Certain types of HPV are known to increase the risk of cancer.
The HPV vaccine
It is recommended that anyone up to age 45 get three doses for long-lasting protection. These doses should be given over a period of 6 months and protect against some of the high-risk types of HPV. Individuals over age 45 may be eligible after speaking with their healthcare provider.
Resources
Meningococcal disease
What is meningococcal disease?
Meningococcal disease is a serious illness caused by a type of bacteria known as Neisseria meningitidis. It can lead to meningitis (infection of the lining of the brain and spinal cord) and infections of the blood. Meningococcal disease often occurs without warning – even among people who are otherwise healthy.
How is it spread?
It can be spread from person to person through close contact (kissing, coughing) or lengthy contact, especially among people living in the same space.
What are symptoms of meningococcal disease?
The symptoms of meningococcal disease vary, but include:
- High fever
- Headache
- Stiff neck
- Vomiting
- Rash
- Sensitivity to light
- Confusion
- Sleepiness
Symptoms may develop in a few hours, but usually over the course of 1 to 2 days. Even when it is treated, meningococcal disease can be deadly. Among those who survive, permanent brain damage, hearing loss, kidney failure, loss of arms or legs, or chronic nervous system problems can occur.
The meningococcal vaccine
The vaccine can help prevent meningococcal disease caused by high-risk types of the bacteria.
HIV-positive people need 2 doses of the vaccine at least 8 weeks apart, followed by revaccination with 1 dose of the vaccine every 5 years.
Several city and state health departments have recommended that residents get vaccinated with 1 dose of the vaccine. Check with your local health department to see if this is recommended in your city.
Resources