Mpox
Updated October 28, 2025
Mpox continues to circulate in 2025. People who are traveling and meeting up in large groups are particularly vulnerable to getting mpox. In October 2025, there are cases of mpox clade 1–a more severe strain–in California. Here’s what you need to know:
- Get two doses of the mpox vaccine–likely for free: If you’ve only had one dose, you should get a second, even if it’s been a while since your first. The vaccines may be available at no cost to you or covered by your health insurance.
- The mpox vaccine is very effective and long-lasting: Studies have shown that two weeks after the second dose, the mpox vaccine is 89% effective. At this time, no public health agencies are recommending more than two vaccine doses, since getting both shots provides long-lasting protection.
- The mpox vaccine is effective against both strains of mpox: Clade 1–the more fatal and infectious strain that caused the 2024 WHO emergency declaration–is prevented along with Clade 2–the strain that was circulating during the 2022 outbreak.
- Pay attention to your body and watch out for symptoms: Even if you have both vaccine doses, if you or a partner spots a new rash or has other symptoms of mpox, get checked out by a doctor or at a local sexual health clinic. This is particularly important right before and after you travel or attend big events (sex parties, bathhouses, clubs).
- Know that hotter hookups start with health: Make sure your STI and HIV testing are up-to-date. Start HIV treatment or HIV PrEP (medicines that prevent HIV). Get info on preventing overdose and grab naloxone (a medication that prevents overdose) and test kits to test any drugs you or your friends may take.
Who is mpox impacting?
Mpox can affect anyone of any gender identity or sexual orientation. However, it’s particularly impacting cisgender men who have sex with men as well as trans people and their sex partners.
Available data suggests that almost half of people diagnosed with mpox in the United States are also living with HIV. The CDC doesn’t know if having HIV increases the likelihood of getting sick with mpox if exposed to the virus.
What are the symptoms?
Symptoms can appear between 5 to 21 days after exposure, and can include:
- An unusual rash or sores, which often start on the face or mouth then spreads to other parts of the body, including your genitals (dick, vulva, testicles), butt (including inside your ass), or inside your vagina/front hole
- Fever
- Headache, muscle aches, and back ache
- Swollen lymph nodes, including in your throat, armpits, and groin
- Chills
- Exhaustion
The rash or sores typically come after the other symptoms listed above, but that is not always the case. Someone can be contagious as soon as any of the above symptoms start. Symptoms can last up to 4 weeks with most people recovering from mild illness within that time.
If you have unusual sores or a rash, get immediate medical attention. You may need to isolate for up to 21 days to prevent passing the virus on to others.
How is the virus spread?
- Mpox is spread through close contact, like touching someone’s rash or sores, and sharing bedding or towels, or through respiratory droplets (kissing, coughing, sneezing).
- It is spread during sex since it often means having close contact, extended time face-to-face and touching someone’s sores on their skin, genitals (dick, vulva, testicles), butt (including inside), inside of a vagina/front hole, or mouth. We don’t yet know if the virus can be spread through semen or vaginal fluids.
- Condoms are not sufficient to prevent mpox transmission. If the rash is only on your genitals or inside your butt, condoms may help reduce the likelihood of developing sores in those areas, which are extremely painful. However, condoms alone are likely not enough to prevent mpox. You still may be exposed if you have skin to skin contact or share bedding/towels.
How can I reduce my risk of infection during sex?
Based on available data about how mpox may be spreading in our community, BHOC has the following suggestions to keep yourself and your sex partners as safe as possible:
- Get vaccinated. CDC data shows that people who did not get vaccinated were 14 times more likely to get mpox than people who did get vaccinated. Find your closest vaccine location and make sure to get BOTH DOSES!
- Ask your sex partners about symptoms and if they’ve been vaccinated with both doses. See if they have had any unusual rashes or sores in the last 3 weeks. Here are some easy ways to ask:
- “I’m down to hookup, but I want to make sure both of us are feeling good since mpox is going around. Have you had any recent rashes or sores?”
- “I want to make sure we are both on the same page with mpox. I haven’t had any new rashes or sores and haven’t been feeling sick. How about you?”
- Stay connected: Even if you’re into anonymous hookups, try to have a phone number or way to get in touch with someone in case you need to reach each other if either of you develop symptoms or get diagnosed with mpox.
- Consider using condoms as a way to avoid painful sores on your genitals: Condoms are not sufficient to prevent mpox transmission. If the rash is only on your genitals or inside your ass, condoms may help reduce the likelihood of developing sores in those areas, which are extremely painful. However, condoms alone are likely not enough to prevent mpox. You still may be exposed if you have skin to skin contact or share bedding/towels. Here are more details on preventing mpox during sex on preventing mpox during sex.
- If you receive a notification from someone you had sex with, take it seriously. Get vaccinated ASAP, which may keep you from developing severe symptoms. Find your closest vaccine location. It also works the other way. If you are diagnosed with mpox, be sure to also let any sex partners know so they can make sure those exposed can get care.
- Notice if you develop symptoms. People are not known to be infectious until they have symptoms; but, keep in mind that someone may have sores in their throat, ass, or vagina/front hole and not know it.
- Stop the spread. If you don’t feel well, take a break from sex. If you live with someone, you may need to isolate yourself from them if you are positive for mpox.
Here’s a video from the CDC on what all sexually-active people should know about mpox:
How can I reduce my risk of infection with other close contacts and at large gatherings?
- Get vaccinated. CDC data shows that people who did not get vaccinated were 14 times more likely to get mpox than people who did get vaccinated. Find your closest vaccine location and make sure to get BOTH DOSES!
- Make informed choices about attending large events. If you’re in large crowds where people are wearing minimal clothing (like at Pride events, saunas, clubs), be aware of how much skin-to-skin contact you may be having. After you attend large group events with lots of skin-to-skin contact, keep an eye out for symptoms, such as a new rash. Here are more details about attending large gatherings.
- If you receive a notification from an event organizer, take it seriously. Find your closest vaccine location ASAP, which may keep you from developing severe symptoms. It also works the other way. If you are diagnosed with mpox, be sure to also let any organizers of events you attended know so they can make sure those exposed can get care.
- Stop the spread. If you don’t feel well, take a break from going out to bars, gyms, clubs, and other events. If you live with someone, you may need to isolate yourself from them if you are positive for mpox.
What should I know about the mpox vaccine?
Find your closest vaccine location and make sure to get BOTH DOSES for the most protection!
There are effective vaccines available for mpox. The vaccines may be available at no cost to you or covered by your health insurance.
Unlike in the past, most places in the U.S. are now offering vaccines to people who have already been exposed to mpox or haven’t been exposed but might be at-risk. See who should get vaccinated at CDC.gov.
Getting vaccinated is important because it:
- Makes getting and spreading mpox less likely.
- Helps to make any symptoms–like proctitis and pain–less severe.
- Reduces your risk of getting seriously ill, being hospitalized, or dying.
There are two different ways the vaccine can be administered: subcutaneously (in the fat under your skin) and intradermally (in a layer very close to the surface of your skin). Those who receive an intradermal vaccine should develop “a noticeable pale elevation of the skin” called a wheal (of which you can see pictures below).

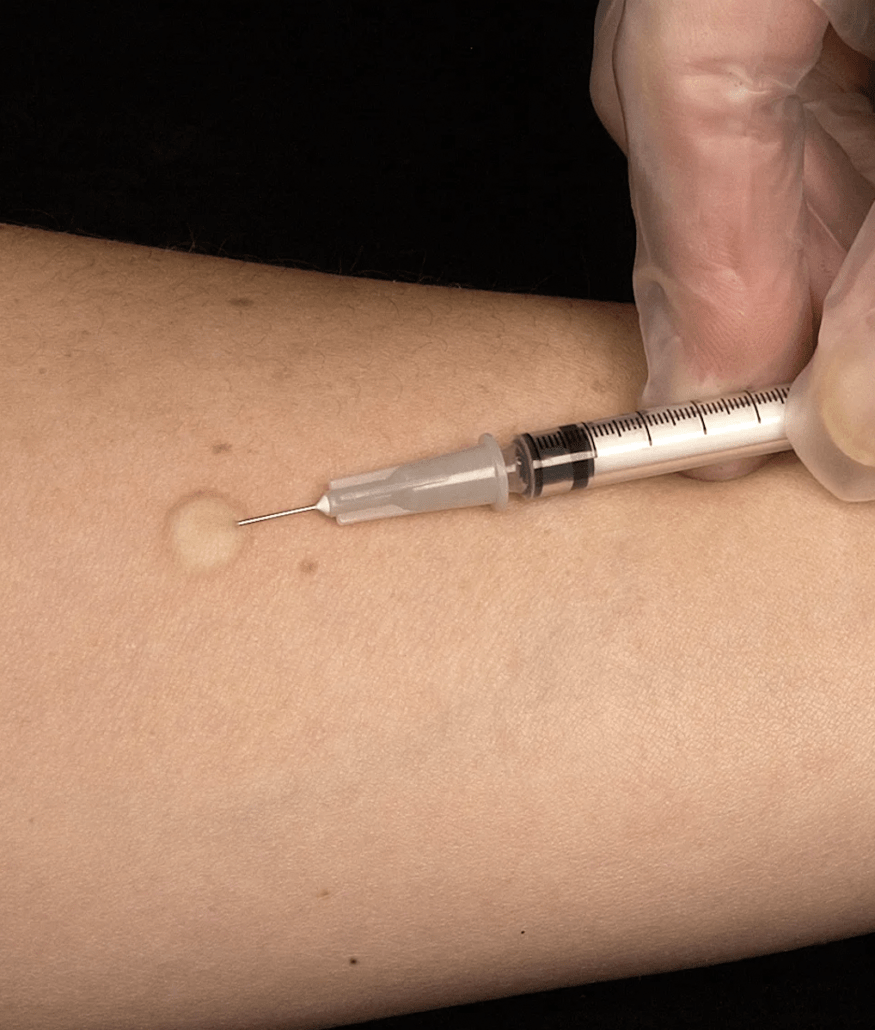
If you don’t want to have a temporary bump or discoloration of skin on your forearm, you can ask your vaccine site about other parts of your body you can receive the injection on. See below.
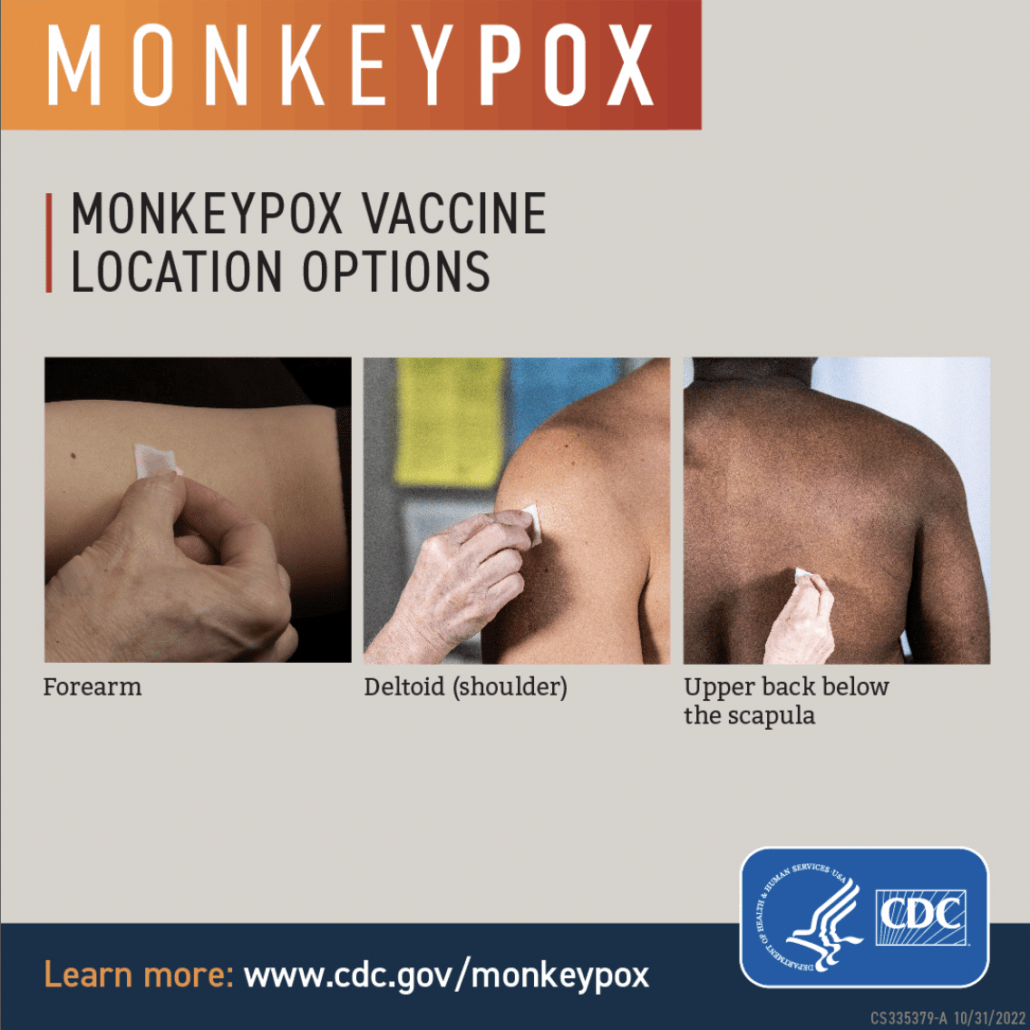
If you have a history of keloid scars or are under 18 years old, you can request a subcutaneous vaccination.
Most people living with HIV will be able to get vaccinated with the Jynneos vaccine. Check with your doctor and send them this CDC guidance in case they might not be up-to-date.
For people who are immunocompromised for any reason, check with your doctor and send them this CDC guidance in case they might not be up-to-date.
If you’ve already had mpox before getting vaccinated, CDC does not recommend you get the vaccine.
When does the vaccine start protecting me?

Vaccines can give you protection from Mpox, but not immediately after you get a shot. Continue practicing harm reduction for the timing shown below when meeting up with others and in your sex life.
If you’ve only received 1 dose of Jynneos:
One dose of Jynneos does offer some protection, but not right away.
- The vaccine needs time to build up your immunity.
- Waiting a few weeks is more protective than waiting a few days.
- After this time period, even one dose of the vaccine is 75% effective at preventing mpox.
- Getting two doses of the Jynneos vaccine will give you the most protection from mpox.
If you’ve received 2 doses of Jynneos:
People are considered fully vaccinated about 2 weeks after their second shot of JYNNEOS. After this time period, having both doses ion the mpox vaccine is 89% effective at preventing mpox.
If you’ve had ACAM2000:
People are considered fully vaccinated about 4 weeks after receiving ACAM2000.
Can vaccinated people still get mpox?
Infections after vaccination are possible. No vaccine, including those for COVID and flu, are 100% effective at preventing illness. Getting vaccinated is important because it:
- Makes getting and spreading mpox less likely.
- Helps to make any symptoms–like proctitis, issues with urination, and pain–less severe.
- Reduces your risk of getting seriously ill, being hospitalized, or dying.
Here’s more information that CDC is updating as of September 2024.
Do I need to get a booster shot after I am fully vaccinated?
At this time, the CDC is not recommending additional vaccines or boosters. If you have received both doses of Jynneos, you have done all you need to to get the most protection from mpox. Make sure to tell your friends and sex partners to get vaccinated as soon as they can!
There will be more information in the future about additional vaccines or boosters so be sure to check CDC.gov for updates.
Can people who have had mpox in the past get mpox again?
At this time, the CDC has said that having mpox likely offers immunity from a future infection. However, research is still ongoing. At this time, the CDC is not recommending vaccination for people who have received an mpox diagnosis in the past. There will be more information in the future about additional vaccines or boosters so be sure to check CDC.gov for updates.
Can I get tested for mpox?
If you have a rash or other symptoms of mpox, you should get tested even if you have been vaccinated or had mpox. The CDC has more information on what to expect when you get tested.
Some other infections–like syphilis, herpes, and HIV–may also cause a rash. When you get tested for mpox, your healthcare provider may also test you for STIs. If you’re sexually active, get tested every 3 to 6 months for STIs and anytime you have symptoms of an infection, like discharge, urinary pain, fever, and more.
When should I get medical attention?
If you or any close contacts (from the last 21 days) have unusual sores or a rash, go see a healthcare provider either at:
- A local clinic (find your closest one here) OR
- With your healthcare provider.
Remind your provider that mpox is circulating. Sometimes the rash and sores can be confused with sexually-transmitted infections, like herpes and syphilis.
If you currently have mpox but are dealing with severe pain and/or belong to a vulnerable community, you may benefit from treatment (TPOXX).
What is the treatment for mpox?
- If someone told you that you have been exposed to mpox, go get vaccinated ASAP, which may keep you from developing severe symptoms. Find your closes vaccine location.
- If you have been diagnosed with mpox and currently have sores, are experiencing pain, issues with using the bathroom (bowel movements and peeing), or other discomfort, you can ask a healthcare provider for TPOXX, an antiviral medication that helps reduce severe symptoms.
Here’s how to do that:- Let your provider know that the CDC updated guidance since the 2022 mpox outbreak to make TPOXX medication much easier to access.
- Providers can fill out the required EA-IND forms after you begin treatment.
- Virtual appointments are allowed to get prescriptions for TPOXX.
- If a provider refuses to prescribe TPOXX, ask them to document their refusal of treatment in your medical chart. If possible, also send a message after your appointment to your provider (either through voicemail or a patient portal) summarizing the visit, including the refusal of treatment.
Who should I tell about my mpox symptoms or diagnosis?
Testing positive for anything–whether it’s an STI, COVID, or mpox–can feel heavy or scary. One of the most important things you can do if you get diagnosed with mpox is to tell your sex partners, people you live with, or anyone else you’ve had prolonged, close contact with from the last 3 weeks. That way, they can get tested, potentially receive treatment, and isolate to prevent passing it on. Here are some people you may need to tell:
- Sex partners
- Partners you live with, roommates, or family members in your household
- Owners or organizers of parties, bars, clubs, events, or bathhouses that you’ve attended
- Sex work clients or anyone you had survival sex with
- Other people who you have had close contact with
Here are some ways to talk about it if you want to send a text or message someone about your positive result. Your healthcare provider you see may also want the information about your close contacts so they can follow up with them as needed.
What happens if I get diagnosed with mpox and have a detectable HIV viral load, am older, or am immunocompromised?
For people who have a weaker immune system, mpox symptoms can last longer and you may experience a longer recovery. You also might also be contagious to others for a longer period of time. Go to your healthcare provider to get support.
CDC has more details on what mpox means if you’re living with HIV which may answer many of your questions. At this time, people living with HIV who are taking their medication and are undetectable are not considered at higher risk for prolonged infection of mpox or any other complications related to the mpox virus.
People living with HIV who are not taking HIV medications are at higher risk for these complications.
People living with HIV and people who are immunocompromised could still benefit from treatment (TPOXX). Talk to your healthcare provider about any potential drug interactions.
What can I do to support the mpox response?
- Get fully vaccinated–both doses–as soon as you can. Find your closest vaccine location
- Report any vaccine side effects (including if you didn’t have any) to the CDC using V-Safe.
Resources
As we learn more, we will be updating this page. For more detailed information, check out your state or local health department’s website and the CDC.
Additional Resources
- Safer Sex, Social Gatherings, and Mpox (CDC)
- Video: 5 Things Sexually Active People Need to Know about Monkeypox (CDC)
- Info on Mpox vaccines (CDC)
- Mpox info for people living with HIV (CDC)
- Global Mpox Info for Queer People (The Love Tank)
- PoxApp: Mpox virus symptom checker (Stanford University)
